Section 7: Mammography
Introduction
This chapter provides information on the requirements and procedures for quality assurance testing of mammographic x-ray machines.
Note that the Canadian Standard of Mammographic Imaging and Technical Quality is set by C.A.R. (Canadian Association of Radiologists).
The following are mandatory tests required to be performed every six months (or as specified) under the HARP Act.
Mandatory HARP Tests
Patient Entrance Exposure
Half-value Layer
Collimation
Automatic Exposure Control
Sensitometry (daily, using mammographic film)
Image Quality (weekly)
|
The following tests are recommended to be performed every six months in addition to the mandatory tests.
Recommended Technical Tests
Output Reproducibility
Timer/mAs Linearity
kVp Accuracy
Film Screen Contact
Compression Device
|
In keeping with current standards of practice, the following tests/procedures are recommended to be performed at the frequency specific to a facility. The frequency of these tests will depend on workload, general condition of equipment, etc. . .
Additional tests
Darkroom cleanliness
Darkroom Fog
Fixer Retention
Viewing Conditions
Support Device Transmission
Grid/Uniform Phantom Image
Focal Spot
Film/Screen Speed
|
Patient Entrance Exposure
Standard
Section 8 (11) of the HARP Regulation states:
"Every medical radiation protection officer, every chiropractic radiation protection officer, and every chiropodic radiation protection officer shall ensure that at the facility where the officer acts, the entrance exposure of that part of a patient set out in Column 1 of Table 6 of a thickness set out opposite thereto in Column 2 of Table 6 that is a distance from the x-ray source set out opposite thereto in Column 3 of Table 6 does not exceed the exposure set out opposite thereto in Column 4 of Table 6."
Table 6
10
|
ITEM |
COLUMN I |
COLUMN 2 |
COLUMN 3 |
COLUMN 4 |
| |
Projection Mammogram |
Patient Thickness |
Source to Image Distance |
Maximum Mean Glandular Dose (mGy) |
|
1. |
(a) Film/DX Receptor |
4 cm (comp) |
As used |
3 mGy |
10editor: Table 6 is abridged to present mammography PEE limits only and to reflect 2001 changes to the HARP Act setting Mean Glandular Dose as the regulated dose parameter.
Equipment
- Radiation dosemeter
- Tape measure
- A mammography image quality and dose equivalent phantom(s). PEE is based on a phantom equivalent to an average 4 cm. compressed breast.
Procedure
Note: This set up will also be used for testing the functions of the Automatic Exposure Control system and reproducibility in the AEC mode.
- Place the mammography phantom on the breast support device. The phantom must be properly orientated and aligned with the chest wall edge of the support device.
- Place the chamber of the dosemeter immediately to the right of the phantom as per figure 1.
- Adjust the position of the automatic exposure control sensor to the centre of the phantom.
- Lower the compression device and apply full compression.
- Select the most commonly used technique for an average 4 cm compressed breast.
- Place a loaded cassette in the cassette holder.
- Take an exposure and record the skin exposure.
- Use the tables located at the following link to calculate the Mean Glandular Dose based on the HVL and the skin entrance exposure.
Mean Glandular Dose Calculator
Note: PEE must be reported at 4 cm above the breast support device. Use the inverse square law to determine the PEE at 4 cm above the breast support device.
Evaluate as follows:
- All PEEs must be below the Ontario limit of 3 mGy.
- Any PEE above the Ontario limit must be reduced immediately.
- Any PEE near the limit should be investigated with a view toward reduction.
Figure 7-1 Mammography Test Setup

Exposure Reproducibility
Standard
Section 13 (2) of the HARP Regulation states:
"Every diagnostic x-ray machine shall be so constructed that,
(ii) each of the ten radiation exposure referred to in subclause (i) is within 20 per cent of the mean value of the ten measurements.
(Over the normal range of use)"
Section 18 (4) of the HARP Regulation states:
"Every x-ray machine that is constructed or adapted to perform mammographic examinations shall be so constructed or adapted that,
(a) for any selected combination of kilovoltage, current and time, the coefficient of variation of any ten consecutive radiation measurements taken at the same distances within a time period of one hour is not greater than 0.08."
Reproducibility in the Automatic Exposure Mode
Procedure
1. Set up the test equipment according to the directions provided in the general setup for PEE measurements. See Figure 7-1.
2. Select the exposure technique which the facility most commonly uses to image a 4 cm compressed breast in Automatic Exposure Control mode.
Note: This test must also be repeated in the manual mode.
3. Make ten exposures and record the output of each of the exposures. 11
11 Allow sufficient time between exposures for the tube to cool. Refer to each x-ray tube's heat rating chart.
Generally, for routine HARP testing which is performed every six months, reproducibility testing can be limited to three exposures. This should be enough information to reveal whether there is a reproducibility problem.
If a problem is suspected, then a complete test must be performed (10 exposures) and calculate the coefficient of variation as well as ensuring that each of the 10 measurements are within 20% of the mean value of the 10 measurements.
See General Radiography - Section 4 for a description of the coefficient of variation formulae and example.
Evaluate as follows:
Reproducibility of the output of an x-ray unit must meet the HARP Regulation's standard described above.
If the x-ray unit does not meet standard then the unit must not be used until it is serviced and retested.
Automatic Exposure Control Tests
Equipment
- Dosemeter
- Mammography phantom
- Aluminum Sheets or different thicknesses of Lucite
- Lead Sheet
Procedure
Set up as per PEE measurements. See Figure 7-1.
The following is a list of tests which must be performed every 6 months or upon servicing of the x-ray equipment to ensure proper automatic exposure control response:
1. Reproducibility of exposure in the automatic exposure control mode. Described earlier in this chapter.
2. Change in density selection.
3. Changes in kilovoltage selection.
4. Changes in milliamperage selection (if applicable).
5. Changes to variance in patient thickness.
6. Back-up System 12, ensure that it is limited to 2000 mAs and that a Back-up timer indicator is present when Back-Up time is reached.
12The back-up system must be tested during an acceptance test at the time of initial installation.
The procedure for testing automatic exposure control system is provided in detail in Automatic Exposure Control -- Section 5.
Evaluate as follows:
The automatic exposure control system is functioning properly if the resulting film optical density is maintained as technique parameters are varied. Items 2 and 6 listed above will result in changes to optical density.
Image Quality Test
Frequency
It is recommended that this test be performed weekly.
Equipment
- Image quality phantom (containing pathological artifacts)
- Loaded cassette (18 cm x 24 cm)
Procedure
- Place the mammography phantom on the breast supporting device. The phantom must be properly orientated and aligned with the chest wall edge of the support device.
- Adjust the position of the automatic exposure control sensor to the center of the phantom.
- Lower the compression device and apply full compression.
- Place a loaded cassette in the image receptor holder.
- Select the most commonly used technique for an average 4 cm compressed breast. Note: With some phantoms the technique may need to be adjusted.
- Make an exposure.
- Process the film using the standard mammography cycle.
- Assess the film under proper viewing conditions.
Evaluate as follows:
- This test film indicates the imaging capabilities of the x-ray unit system, film/screen and processing.
- Each facility should set their own tolerances or follow the manufacturer's guide.
- Evaluate the film for the number of artifacts seen. Record and compare the results with that from the previous week. Ensure that the results are consistent.
Note:
Based on the RMI 156 phantom, the X-ray Inspection Service requires that the following artifacts are clearly visible on the phantom image.
|
Artifact |
Standard |
|
Microcalcifications |
0.32 mm |
|
Fibres |
0.75 mm |
|
Masses |
1.00 mm |
Reproducibility (Manual Mode)
Standard
Section 13 (2) of the HARP Regulation states:
"Every diagnostic x-ray machine shall be so constructed that,
(ii) each of the ten radiation exposure referred to in subclause (i) is within 20 per cent of the mean value of the ten measurements."
(Over the normal range of use)
Section 18 (4) of the HARP Regulation states:
"Every x-ray machine that is constructed or adapted to perform mammographic examinations shall be so constructed or adapted that,
(a) for any selected combination of kilovoltage, current and time, the coefficient of variation of any ten consecutive radiation measurements taken at the same distances within a time period of one hour is not greater than 0.08."
Procedure
- The phantom is removed from the image receptor and the probe of the dosemeter is placed in the middle of the x-ray field, 4 cm. above the breast support device.
- Select a technique that is commonly used in the manual mode or select 30 kVp, 0.2 seconds.
- Take an exposure and record the output (milliroentgens). If possible also note the exposure time (seconds).
- Make ten exposures and record the output of each of the exposures.13
13Allow sufficient time between exposures for the tube to cool. Refer to each x-ray tube's heat rating chart.
Generally, for routine HARP testing which is performed every six months, reproducibility testing can be limited to three exposures. This should be enough information to reveal whether there is a reproducibility problem. If a problem is suspected, then a complete test must be performed (10 exposures) and calculate the coefficient of variation and if each measurements is within 20% of the mean value of the 10 measurements.
See General Radiography - Section 4 for a description of the coefficient of variation formulae and example.
Evaluate as follows:
Reproducibility must meet the HARP regulation's standard described above.
If the x-ray unit does not meet standard then the unit must not be used until it is serviced and retested.
mA Linearity
Standard
Section 13 (4) of the HARP Regulation states:
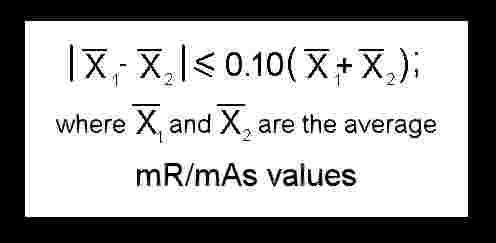
"Where a diagnostic x-ray machine is constructed so that the tube current (in milliamperes) has a range of preset values and both it and the exposure time (in seconds) can be selected individually, the average ratios of exposure (in milliroentgens) to the product of tube current and exposure time, obtained at any two adjacent tube current settings for any fixed indicated value of x-ray tube potential (in kilovolts) over the normal range of use of the machine, shall not differ by more than O.10 times their sum or
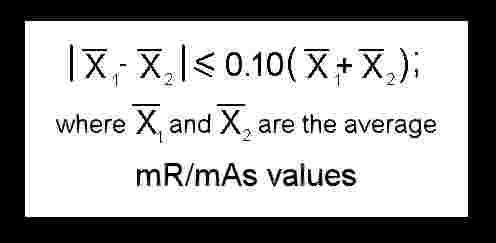 where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliamperes)."
where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliamperes)."
Equipment
- Radiation dosemeter
- Measuring tape
Procedure
Continued from reproducibility testing in the manual mode.
- The phantom is removed from the image receptor and the probe of the dosemeter is placed in the middle of the x-ray field, 4 cm above the breast support device.
- Select a technique that is most commonly used in the manual mode (we suggest 30 kVp; 0.2 seconds).
- Take an exposure and record the output (milliroentgens).
- Select another mA station adjacent to the first mA station. Note, as the mA station is changed, ensure that the kilovoltage remains the same throughout the test.
- Take an exposure and record the output (milliroentgens).
- Repeat steps 4 and 5 until all adjacent mA stations within the normal range of use have been checked.
- Calculate the mR/mAs for each mA station.
Evaluate as follows:
Ensure that the mR/mAs remains constant for all mA stations. If the output is not consistent throughout the test, then you must calculate the mA linearity by using the following formula where x1 and x2 are the average mR/mAs at two adjacent mA stations.
(6) mA Linearity Formula
If linearity does not meet this standard the x-ray unit must be serviced to restore mA linearity and the test repeated after repair.
mAs Linearity (if applicable)
Standard
Section 13 (5) of the HARP Regulation states:
"Where a diagnostic x-ray machine is constructed so that the exposure selection can be
made only as the tube current exposure time product (in milliampere-seconds) or where the milliampere value is continuously variable, the average ratios of exposure (in
milliroentgens) to the product of tube current and exposure time, obtained at any two
selection of milliampere-second differing by at least a factor of two, for any fixed indicated value of x-ray tube potential (in kilovolts) within the range of normal operation of the machine, shah not differ by more than O.10 times their sum or
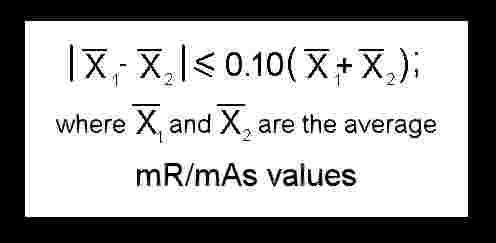 where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliampere-seconds)."
where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliampere-seconds)."
Procedure
The procedure for testing mAs linearity is virtually identical to the testing of mA linearity. Instead of selecting mA stations, mAs selections are used. Starting at 5 mAs, each subsequent setting is doubled until the maximum mAs used is reached.
Follow the procedure as stated for mA Linearity, noting the changes indicated above.
mA Meter Accuracy (if applicable)
Procedure
1. Select 30 kVp and 1 second (to allow time for the mA meter to register).
2. Select mA station normally used.
3. Make an exposure, observe the mA meter and record the value registered by the mA meter.
4. Select another mA station normally used. (Allow tube to cool between exposures.)
5. Make an exposure and record the value registered by the mA meter.
Evaluate as follows:
Assess if the values registered by mA meter are within 50 percent of the selected mA. If the registered values are not within 50 percent of the selected mA values, the mA meter must be serviced.
Half-value Layer
Standard
Section 9 (3) of the HARP Regulation states:
"Every diagnostic x-ray machine shall be provided with,
(b) filters that,
(i) are located in the exit port of the x-ray tube housing or beam limiting device or both,
(ii) intercept the entire useful beam, and
(iii) at a measured potential set out in Column 1 of Table 8 with a thickness of aluminum set out opposite thereto in Column 2 of Table 8, reduce the exposure at least by half."
Table 8
14
|
ITEM |
COLUMN 1
Measured Potential (kilovolts peak) |
COLUMN 2
Half-value Layer (millimetres of aluminum) |
|
1 |
30 |
0.3 |
|
2 |
40 |
0.4 |
|
3 |
49 |
0.5 |
|
4 |
50 |
1.2 |
14Table 8 is abridged to present values applicable to mammography.
Equipment
- Radiation dosemeter
- Aluminum sheets (Type 1100 alloy --at least 4 sheets 0.1 mm thickness)
- Masking tape
Procedure
1. Place the dosemeter 4 cm. above the breast support device in the middle of the x-ray field. The compression device is placed as high as possible and must remain in this position throughout the test.
2. Select 30 kVp and approximately 0.2 seconds in the manual mode. (The time setting should be such that the output is anywhere between 200 to 400 mR.) The target film distance, position of the dosemeter, compression device and technique factors must remain constant throughout the test.
Note:
The half-value layer test is dependent on the kVp accuracy. Therefore, you may wish to verify kVp accuracy before doing this test.
3. Take an exposure and record the output (milliroentgens). This is the zero reading.
4. Tape 0.3 millimetres of aluminum to the face of the collimator or cone. If you wish, you can place the aluminum filters on the compression device. Ensure that the filters completely covers the dosemeter probe.
5. Make an exposure and record this second measurement.
6. Evaluate the two measurements:
c. If the half-value has not been reached then additional filtration must be added to step 4.0. Take another exposure and reassess. Continue adding filtration until the half-value has been reached or exceeded.
d. If the half-value has been reached or passed remove 0.1 mm of filtration from step 4 and take another reading. Continue adjusting the amount of aluminum filtration until the half-value has been reached.
7. Remove all added aluminum sheets in step 4.0 and repeat the zero reading to ensure that the
radiation output has remained constant throughout the test.
8. Calculate the half-value layer (mathematically or by plotting on semi-log paper) and record
the value.
Evaluate as follows:
If the measured half-value layer exceeds the minimum requirement at the measured kVp stated in Table 8, the x-ray machine has sufficient filtration.
If the measure half-value layer is less than the minimum requirement at the measured kVp stated in Table 8, the machine must be serviced. Additional filtration must be added and the half-value layer test repeated.
Note:
In mammography the half-value layer should not be too high. We generally measure it to be around 0.35 to 0.41 at 30 kVp.
Timer Tests
Standard
Section 18(4) of the HARP Regulation states:
"Every diagnostic x-ray machine that is constructed or adapted to perform mammographic examinations shall be so constructed or adapted that,
(b) where the timer is non-mechanical, it is accurate to within 1/30 second (two cycles) or 10 per cent of the set value, whichever is greater; and
(c) where the timer is mechanical, it is accurate to within 1/20 second or 15 per cent, whichever is greater."
Section 11 (1) of the HARP Regulation states:
"Every diagnostic x-ray machine and every fluoroscopic x-ray machine shall, except where the x-ray machine is equipped with an automatic exposure control device, be so constructed that the timing device on the machine terminates an irradiation on completion of'
(a) a preset time interval
(b) a preset product of current and time; or
(c) a preset number of pulses"
Section 11 (3) of the HARP Regulation states:
"Every timing device on a diagnostic x-ray machine and fluoroscopic x-ray machine shall be so constructed that it,
(a) resets automatically to its original position or to ZERO on termination of an irradiation; and
(b) prevents and irradiation from occurring at the ZERO or OFF position."
Section 13 (2c) of the HARP Regulation states:
"Every diagnostic x-ray machine shall be so constructed that,
the timer on the x-ray machine may be set to control irradiations as short as 1/30 second or five milliampere-seconds, whichever is greater."
Equipment
Procedure
1. Place the digital x-ray timer above the breast support device.
2. Select 30 kVp.
3. Make an exposure with time set at the ZERO or OFF position of the timer (if applicable).
4. For each time setting within the normal range of use, expose and record the measured time.
5. After making one exposure at the maximum time setting (within the normal range of use), take a second (partial) exposure but release the exposure switch before the exposure is complete (deadman).
6. Record the measured time.
Evaluate as follows:
If any of the following standards aren't met, the x-ray machine must be taken out of service until such time that is has been serviced and the test repeated to confirm proper functions.
Minimum Exposure Time
The x-ray machine must be able to be set at 1/30 second or 5 mAs.
Timer Inoperative at Zero or Off Position
The x-ray machine must not produce an exposure when the timer is set at the zero or off position. If an exposure is measured, the machine must be immediately taken off-line and serviced.
Timer Accuracy
Measured time must be accurate to within +/- 1/30 second or +/- 10 per cent whichever is greater.
Timer Resets or Zeros on Completion of Exposure
The timer must reset or zero itself after an incomplete exposure. If the machine does not reset or zero, it must be immediately taken off-line and serviced.
Reproducibility
Ensure the timer is reproducible to within a coefficient of variation of 0.08
Deadman
Radiation must stop when the operator releases the exposure switch before the selected time has been reached.
Collimation
Standard
Section 18(1) of the HARP Regulation states:
"Every x-ray machine that is used to conduct mammographic x-ray examinations shall be equipped with,
(a) an x-ray beam limiting device that limits the useful beam so that at any target-toimage-receptor distance specified for the machine the x-ray field in the plane of the image receptor,
(i) does not exceed the edge of the image receptor next to the chest wall by more
than 2 per cent of the target-to-image-receptor distance, and
(ii) except for the edge of an image receptor referred to in subclause (i), does not
extend beyond any other edge of the image receptor. "
Section 18(2) of the HARP Regulation states:
"A removable fixed-operative beam limiting device that is installed on an x-ray machine that is constructed or adapted to perform mammographic examinations shall bear on its external surface clearly visible permanent markings that state,
(a) the image receptor size; and
(b) the target-to-image-receptor distance for which the beam limiting device is designed"
All x-ray units must have:
A. A means to limit the x-ray field to the size of film used.
For systems without a light field indicator, using different size apertures, each aperture must be checked and accurately labelled to indicate the x-ray field size at the film.
For systems with a light field, check that the light field represent the actual x-ray field to within an accuracy of 2% of the target to image receptor distance.
B. A means to limit the x-ray field to the chest wall edge of the image receptor device to within 2% of the target to image receptor distance.
Refer to General Radiography - Section 4 for collimation procedure methods.
Kilovoltage Accuracy
Standard
Section 18(3) of the HARP Regulation states:
"Every mammographic x-ray machine shall be so constructed that the accuracy of kilovoltage calibration for the machine is +/- 1 kilovolts for kilovoltage up to thirty-five and +/- 4 per cent for kilovoltage above thirty-five."
Equipment
Procedure
1. Place the digital kVp meter on the cassette holder and centre it to the x-ray beam. Ensure that the meter is level and that the kVp meter chambers are flooded by the x-ray beam.
2. Select single phase, three phase or constant potential selection as appropriate (if applicable).
3. Measure the kVp at several kVp stations in the range of use.
Evaluate as follows:
The regulation requires kilovoltage accuracy to be within +/- 1 kV for film mammography. Please take meter accuracy into consideration.
Leakage Radiation (if applicable)
Standard
Section 14 of the HARP Regulation states:
"(1) The leakage radiation measured at a distance of one metre in any direction from an x-ray source shall not exceed 100 millirOentgens in one hour under any conditions.
(2) The leakage radiation measurements referred to in subsection (1) shall be averaged over an area of I O0 square centimetres with no linear dimension greater than twenty centimetres."
Equipment
- Survey meter
- 3.0 mm thickness of lead
Procedure
This test need only be performed when there is noticeable damage to the tube housing or when the unit is first installed for acceptance tests.
1. Close the collimator blade completely.
2. Place a 3.0 mm thick piece of lead on a flat surface.
15
15If lead is not available, stack the owner's protective devices.
3. Position the collimator face in close contact with the lead, ensuring that the primary beam is
absorbed by the lead.
4. Select the maximum exposure that is obtainable within tube ratings.
5. Select rate mode on the survey meter and position the instrument, one meter from the focal
spot.
6. Expose and record leakage radiation.
7. Measurements at 5 positions are necessary for leakage assessment:
a. 1 metre anteriorly from the focal spot
b. 1 metre posteriorly from the focal spot
c. 1 metre laterally from each side of the focal spot
d. 1 metre above the focal spot
Evaluate as follows:
Repair or replace the x-ray tubehead if at any point the leakage reading is greater than 100 milliroentgens in any one hour.
Support Device Transmission
Standard
Section 18(lb) of the HARP Regulation states:
"An image receptor supporting device that is shielded sufficiently to ensure that for each activation of the x-ray tube the radiation exposure does not exceed 0.1 milliroentgen where,
(i) the machine is operated,
(A) in the mammographic mode,
(B) at the maximum rated x-ray tube potential
(C) the maximum rated tube current-exposure product for that tube potential and
(D) at the minimum target to image distance attainable and
(ii) the radiation exposure is averaged over a detection area of l00 square centimetres,
with no linear dimension greater than twenty centimetres and centered attire centimetres from an accessible surface beyond the plane of the support device."
Equipment
- Survey meter with a 180 cc (scatter probe)
Procedure
This test is only required when the x-ray unit is first installed for acceptance tests or when there is noticeable damage to the breast support device.
1. Select the maximum kVp available and maximum mAs. (Follow the tube rating chart)
2. Select the minimum target-to-image distance attainable.
3. Position the scatter probe 5 cm below the breast support device and centre it to the x-ray field.
4. Take an exposure and record the reading.
Evaluate as follows:
If the reading is below 0.1 mR no further testing need to be done.
If the reading is at or above 0.1 mR., move the probe 5 cm laterally and take another reading. Average the two readings. If the average is at or above 0.1 mR then steps must be taken to service the breast supporting device to eliminate radiation passing through it.
Compression Device
Standard
Section 18 (1c) of the HARP Regulation states:
"Every x-ray machine that is used to conduct mammographic x-ray examinations shall be equipped with a device that will compress the breast of the patient being x-rayed"
Procedure
All mammographic x-ray unit must have a compression device.
It should be easily adjustable and must be stable when locked into its desired position so that the compression plate does not wobble or move.
The compression device should also be tested routinely for it's force to avoid accidental over compression.
This can be tested using a bathroom or spring scale. The compression force should range from 25 to 40 pounds.
**WARNING**
DO NOT allow your compression device to exceed 45 lb.
This could damage the device and may interfere with the grid motion of the bucky.
Photographic Quality Assurance
Darkroom Fog
The Darkroom must be checked routinely for Darkroom fog. In complete darkness, take a film out of the box, preferably a new box of film, and expose this film with the sensitometer on each long edge of the film. Place this film on the counter top in the usual work area in Darkroom. Cover half the film with an opaque cardboard. Tum on the safelights as normally used and wait 2 minutes, then develop the film.
Measure the density at several steps on the side of the masked film and compare this to the masked side. If the difference is more than 0.02 density units, it is unacceptable and the further test should be done to determine the source of problem and corrected.
This test should be carried out every 6 months or when a problem is suspected.
Darkroom Cleanliness
As mentioned earlier, dust can produce artifacts on a mammographic film. Thus the Darkroom should be cleaned daily, particularly countertops and the processor feed tray. If there is any evidence of static on the films, the Darkroom should be humidified.
Fixer Retention
This should be done quarterly, using a solution of water, acetic acid and silver nitrate. A drop of solution is placed on a developed film and allowed to stand for 2 minutes. Compare this spot to the commercial chart, assess fixer retention and follow the manufacturer's direction.
Viewing Conditions
The viewing room should be dimly lit or illuminated only by light passing through the film. The ambient light level in the viewing area should not exceed 86 lux.
Wherever possible, portions of the view box that are not covered by mammogram films should be masked with black cardboard or fully exposed film. The luminance of each view box should be at least 5500 lux with less than 10% variation across the surface. Whenever a lamp in a viewer needs replacing, the entire set of lumps should be replaced to maintain a uniform intensity and colour across the viewing area. Cool white or daylight rather than warm white tubes are recommended. 16
16 G. Mawdsley, M. Yaffe, Ontario Breast Screening Program, Quality Control in Mammography, 1992.
Grid/uniform Phantom Images
This test is to verify that the density is even throughout the film. At the same time you can use this film to assess for grid lines and verify for consistent performance of the x-ray system.
It is recommended that this test be done weekly.
Take a radiograph of acrylic sheet(s) equal to approximately 4 cm in thickness and big enough to cover the x-ray film. Once a technique is chosen for "average" patients, that technique should be used to expose the acrylic phantom on a weekly basis.
The Optical density of these films should be within 0.2 of the standard Optical density. This will show that the mR/mAs, kVp, filtration and processing speed have not varied significantly. If a change greater than 0.2 is seen, the source of the problem must be detected and corrected. The density must be even throughout the film. If the density varies by more than 0.2 from one area on the film to another, the source of the problem must be detected and corrected. If grid lines are very prominent, the source of the problem must be detected and corrected
Screens
Cassettes and screens should be cleaned at least weekly. In many practices with high patient workloads, daily screen cleaning is necessary. This should be performed at the end of the workday, so that the screens will have time to air-dry overnight.
Film/screen contact should be performed every 6 months using a copper mesh with 30 - 40 wires-to-an inch mesh. This test measures the uniformity of contact between the screen and the film. Poor contact can reduce resolving power. Cassettes that are not correctly closed can allow air trapping and result in poor screen-film contact. The decrease in sharpness from poor screenfilm contact may be such that the films are not obviously blurred, but the fine microcalcifications could go undetected.
The contact test tool is placed directly on a loaded cassette that has been placed on top of the image receptor or breast support device. Expose the film at 28 kVp with an appropriate mAs. Process the film.
Check the film for any dark spots in the mesh area (poor contact, appears as dark spots) or for blurry areas.
Pass
1. No areas of increased density are seen on the radiograph.
2. Two or three areas of increased density _< 1 cm in diameter where tissue is most likely to be
imaged.
3. Multiple random areas of increased density, but all areas are less than 1 cm in diameter.
Fail
1. One or more areas of increased density on the film greater than 1 cm in diameter and located
anywhere tissue is generally images.
2. Four or more areas of increased density 1 cm in diameter, especially near the chest wall side
of the cassette.
Cassettes require a relaxation period of about 15 minutes between loading and use to allow air trapped between the screen and film to escape and allow better contact and resolution. This waiting period should also be allowed before making a clinical exposure.
Film/screen Uniformity of Patient Entrance Exposures
The film/screens should be evaluated for uniformity of speed by exposing each of them to a fixed exposure with a uniform phantom. Verify that all films have densities matching to within 0.15 optical density.
Focal spot
This test should be done when acceptance tests are done or whenever a problem arises were focal spot size deterioration is suspected.
The recommended method for measuring focal spot size is magnification imaging of the focal spot using a pinhole of slit camera.
Measure the focal spot size and ensure it meets the IEC/NEMA standards. (International Electrotechnical Commission/National Electrical Manufacturers Association).
Note:
The star pattern (0.5 degree) can be used for a quick quality control check on the focal spot size. The measurement may underestimate the true size by up to 50%. However, results are reproducible and can be compared if test images are kept throughout the life of the equipment.


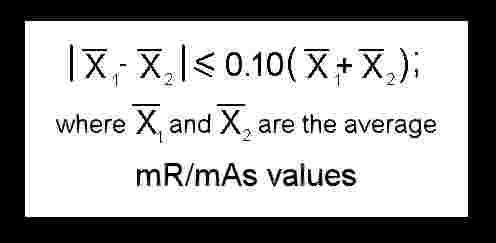 where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliamperes)."
where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliamperes)."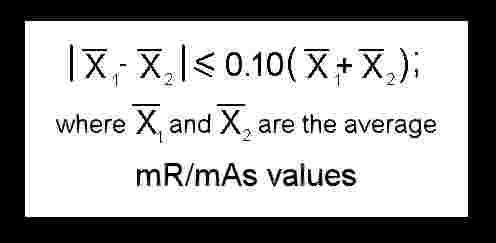 If linearity does not meet this standard the x-ray unit must be serviced to restore mA linearity and the test repeated after repair.
If linearity does not meet this standard the x-ray unit must be serviced to restore mA linearity and the test repeated after repair.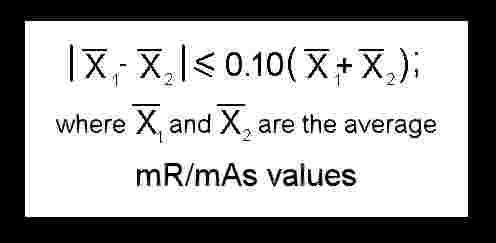 where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliampere-seconds)."
where x1 and x2 are the average mR/mAs (milliroentgens divided by milliampere-seconds) values obtained at the two selected settings of mA (milliampere-seconds)."